|
Magnesium is an essential mineral involved in numerous biochemical processes in the body. It's available in various forms, each with distinct properties and uses. Here's a detailed look at the different forms of magnesium:
1. Magnesium Citrate
What About Magnesium Chelate? Magnesium chelate refers to a form of magnesium that is bound to an organic molecule, typically an amino acid. The chelation process helps enhance the absorption and bioavailability of magnesium in the body. Here’s a closer look at magnesium chelate: Magnesium Chelate1. What is Magnesium Chelate?
3. Benefits of Chelated Magnesium
0 Comments
Hello, health-conscious readers! Today, we're embarking on a journey to unlock the secrets of liver health. Your liver, often referred to as your body's silent hero, performs vital functions that keep you thriving. But did you know that its well-being is closely linked to your gut health? In this friendly yet scientific exploration, we'll delve into the world of liver health, understand the gut-liver connection, and learn about liver-loving foods, lifestyle habits, and supplements that can keep your liver in top shape. The Remarkable Liver: Your Body's Multitasker Before we delve into the connection between the liver and gut health, let's take a moment to appreciate the liver's incredible role in your well-being. This resilient organ has a variety of functions, including filtering blood, metabolizing nutrients, and detoxifying harmful substances. It's the ultimate multitasker, and it deserves our attention and care. The Gut-Liver Connection: A Vital Link Now, let's explore the intricate relationship between your gut and liver: Nutrient Absorption: Your gut is responsible for absorbing nutrients from the food you eat. These nutrients are then transported to the liver for processing and distribution throughout the body. A healthy gut ensures that the liver receives the essential components it needs to function optimally. Detoxification: The liver is your body's primary detoxifier, neutralizing toxins and waste products. A well-balanced gut microbiome can aid in detoxification by breaking down harmful substances before they reach the liver. Inflammation Control: An unhealthy gut can lead to chronic inflammation, which can affect the liver. Inflammation in the gut can trigger a similar response in the liver, potentially leading to liver damage over time. Liver-Loving Foods: Nutrient-Packed Choices Now, let's dive into the first part of our liver health strategy--choosing the right foods: Leafy Greens: Foods like spinach, kale, and Swiss chard are rich in antioxidants that support liver function and protect it from oxidative stress. Steaming before eating can help with digestion and minimize oxalates. Cruciferous Vegetables: Broccoli, cauliflower, and Brussels sprouts contain compounds that aid detoxification processes in the liver. Fiber-Rich Foods: Whole grains, legumes, and fruits provide dietary fiber that aids digestion and helps remove waste products from the body, reducing the liver's workload. Healthy Fats: Avocados, fatty fish (like salmon), and nuts are excellent sources of healthy fats that can help reduce liver inflammation. Liver-Healthy Lifestyle Habits: Good Choices for Well-Being Now, let's explore the second part of our strategy--adopting liver-friendly lifestyle habits: Stay Hydrated: Drinking plenty of water helps the liver flush out toxins and metabolic waste, ensuring it operates efficiently. Limit Alcohol: Excessive alcohol consumption can harm the liver. If you drink, do so in moderation to protect this vital organ. Regular Exercise: Engaging in regular physical activity helps maintain a healthy weight and reduces the risk of fatty liver disease. Stress Management: Chronic stress can impact gut health and, in turn, liver health. Incorporate relaxation techniques like meditation or yoga into your routine to keep stress in check. Beneficial Liver Supplements: Enhancing Your Liver's Health Finally, let's explore the third part of our strategy—considering beneficial liver supplements: Milk Thistle: Supplements containing silymarin, found in milk thistle, are known for their potential liver-protective properties. Vitamin E and C: These antioxidants can support liver health by protecting it from oxidative damage. Omega-3 Fatty Acids: Found in fish oil supplements, omega-3s can help reduce liver inflammation and improve fat metabolism. Consult a Professional: Before adding any new supplements to your routine, consult with a Functional Medicine Practitioner to ensure they are appropriate for your specific needs and health status. Your Liver, Your Lifelong Ally In this article, we've uncovered the vital role of the liver in maintaining your overall well-being. Remember, a healthy liver starts with a well-balanced gut, supported by liver-loving foods, lifestyle habits, and supplements. By nurturing your liver from gut to good habits, you're investing in a healthier, more vibrant future. Here's to a thriving liver and a vibrant life! As you navigate this path, know that I'm here to provide guidance, insights, and evidence-based strategies to help you unlock the potential of your gut for vibrant living. Your initial consultation is free and you can request it by clicking the button below: Not ready for a consultation? Want to learn more about how to support your liver health? Download our free Liver Health Guide Below.
Hello, my fellow readers! Today, we're diving deep into a topic that concerns many of us – hair loss. Our hair, a visible marker of our health and vitality, is more than just a part of our appearance; it's a reflection of our well-being. But did you know that the root of hair health might just lie in an unexpected place—the gut? In this article, we'll uncover the gut-hair loss connection, understand how nurturing your gut can lead to healthier hair, and explore strategies for maintaining a luscious mane.
The Fascinating World of Hair Loss First, let's get acquainted with hair loss, a concern that affects millions worldwide. Scientifically termed "alopecia," it can occur for various reasons, from genetics to hormonal imbalances. While it's a common issue, it's not one you have to accept without exploring potential solutions. The Gut: Beyond Digestion Now, let's shift our focus to the gut, a dynamic system that's often overlooked in its complexity. Beyond its primary role in digestion, the gut is home to a vibrant community of microorganisms, plays a pivotal role in immune system coordination, and even influences our hormonal balance. And yes, it turns out that a happy gut can lead to happier, healthier hair. The Gut-Hair Loss Connection: Unveiling the Secrets Nutrient Absorption: The gut is responsible for absorbing essential nutrients, including those vital for hair health. Nutrients like biotin, zinc, and iron are crucial for strong, vibrant hair. An unhealthy gut can hinder the absorption of these nutrients. Inflammation: A compromised gut can trigger chronic inflammation, which can disrupt hair follicle function and lead to hair loss. Conditions like alopecia areata have an inflammatory component. Hormonal Balance: Hormonal imbalances, often linked to the gut, can affect hair growth cycles. For example, elevated levels of the hormone dihydrotestosterone (DHT) are associated with male and female pattern baldness. Stress Response: The gut and the brain are closely connected through the gut-brain axis. Stress, which can negatively impact gut health, can also contribute to hair loss by pushing hair follicles into a resting phase. Caring for Your Gut and Hair Now that we've unveiled the gut-hair loss connection, here are some friendly scientific tips to promote hair health through a happy gut: Diet: Prioritize a balanced diet rich in essential nutrients like biotin, zinc, iron, and antioxidants. Consume foods like eggs, nuts, leafy greens, and fruits to support both gut and hair health. Probiotics: Consider incorporating probiotics into your diet to promote a healthy gut microbiome. Yogurt, kefir, and fermented foods like sauerkraut are excellent choices. Stress Management: Practice stress-reduction techniques like meditation, yoga, or deep breathing exercises to keep your gut-brain axis in harmony. Adequate Hydration: Stay hydrated to support overall well-being, including hair health. Consult a Specialist: If you're concerned about hair loss or gut issues, consult a functional medicine practitioner who specializes in both areas. They can test for hormones, viral and bacterial overgrowths as well as liver health to provide tailored advice and solutions. In this article, we've uncovered the fascinating connection between gut health and hair loss. Remember, a nourished gut can be the foundation for healthier hair. By nurturing your gut through a balanced diet, stress management, and professional guidance, you're taking proactive steps toward maintaining a luscious and vibrant mane. Here's to strong, beautiful hair and a thriving gut! As you navigate this path, know that I'm here to provide guidance, insights, and evidence-based strategies to help you unlock the potential of your gut for vibrant living. Your initial consultation is free and you can request it by clicking the button below: Inside our cells, there's a hidden world of energy production that keeps us going, from simple tasks like breathing to complex thinking processes. Imagine it as a dynamic dance of vitality, all choreographed by tiny cell powerhouses called mitochondria. In this journey, we'll skip the heavy scientific jargon and explore the wonders of cellular energy, demystify the role of mitochondria, and unveil how your gut health can help you conquer the enigmatic Chronic Fatigue Syndrome (CFS).
Mitochondria: Your Cellular Energy Factories Meet mitochondria, your cell's energy factories. They're like the engines powering your body. These microscopic structures, found within our cells, work their magic through a process called oxidative phosphorylation. Think of it as a little powerhouse that churns out energy in the form of adenosine triphosphate (ATP), which is the fuel for everything your body does. Mitochondrial Hiccups in Chronic Fatigue Syndrome Now, let's talk about Chronic Fatigue Syndrome (CFS). It's like that uninvited guest at a party, and it brings persistent and unexplained fatigue. Researchers have been working hard to understand it better. What they've found is intriguing - it looks like the energy factories (mitochondria) aren't working as they should. Imagine a factory with a glitchy assembly line, that's what's happening with ATP production in CFS. It's slower and less efficient. The Intriguing Gut-Mitochondria Connection Now, let's explore the intricate interplay between gut health and mitochondrial function: Nutrient Absorption: The digestive system, notably the small intestine, serves as the portal for nutrient absorption. Essential cofactors such as coenzyme Q10 (CoQ10) are absorbed here, critical for mitochondrial function. However, other nutrients are equally pivotal, including B-vitamins (especially B2, B3, B5, B6), magnesium, and iron. Microbiome Influence: Our gut microbiome, a bustling community of trillions of microorganisms, plays a pivotal role in gut health. Emerging research indicates that the composition and activities of these microbes can influence mitochondrial function. Dysbiosis, an imbalance in gut microbiota, may contribute to mitochondrial dysfunction and CFS. Inflammation and Oxidative Stress: Dysbiosis and gut permeability issues can trigger chronic inflammation and oxidative stress within the gut. These systemic responses can have a detrimental impact on mitochondrial health. It's worth noting that inflammation and oxidative stress are also influenced by antioxidant-rich foods. Mitochondrial Biogenesis: New evidence suggests that molecules and signaling pathways originating in the gut may influence mitochondrial biogenesis. This process, responsible for creating fresh mitochondria, is pivotal for sustained cellular energy production and overall vitality. Nurturing Your Gut for Enhanced Cellular Energy To fortify your gut health and optimize mitochondrial function, consider these comprehensive strategies: Diverse Diet: Embrace a well-balanced diet rich in fiber, prebiotics, and probiotics to cultivate a flourishing gut microbiome. Incorporate foods high in CoQ10, such as organ meats and spinach, but also include a variety of nutrient-rich foods like legumes, whole grains, leafy greens, and lean meats to ensure you receive a spectrum of essential nutrients. Supplementation: Consult with functional nutrition professionals to explore targeted supplements for mitochondrial support. These may include CoQ10, B-vitamins, magnesium, and iron, depending on individual needs and deficiencies. Stress Mastery: Chronic stress exacts a toll on gut health and mitochondrial vitality. Prioritize stress management through meditation, mindfulness, regular physical activity, and ample sleep. Holistic Care: Seek guidance from healthcare specialists who specialize in CFS, mitochondrial disorders, and gut health. Individualized approaches and expert consultation are paramount when navigating the intricate landscapes of these complex health issues. The connection between gut health, mitochondrial energy production, and conditions like Chronic Fatigue Syndrome continues to unveil itself as an exciting frontier in cellular biology and functional medicine. This comprehensive exploration has illuminated the profound role our gut plays in sustaining mitochondrial vitality, influencing our overall well-being. By implementing the strategies outlined above, and by staying informed about cutting-edge research, you can embark on a journey toward the optimal maintenance of cellular energy and holistic health. Keep in mind that the path to well-being is individualized, and collaborating with a functional medicine practitioner remains paramount when addressing complex health issues like CFS, mitochondrial dysfunction, and gut health. As you navigate this path, know that I'm here to provide guidance, insights, and evidence-based strategies to help you unlock the potential of your gut for vibrant living. Your initial consultation is free and you can request it by clicking the button below: Greetings, fellow health enthusiasts! Today, we're embarking on a journey into the realm of joint health, where the vitality of our joints, like the cogs in a well-oiled machine, keeps us moving. But here's the twist - our gut, often considered the epicenter of our overall well-being, may play a more pivotal role in joint health than you might think. In this friendly but scientific exploration, we'll dive into the world of joints, unravel the gut-joint connection, and understand how nurturing your gut can lead to happier, more flexible joints. The Remarkable World of Joints Joints, those marvelous connections between bones, are integral to our daily activities, from bending to stretching, walking to running. They come in various shapes and sizes, but they all have one thing in common: the need for proper care. The scientific term for joint health is "arthrology," and it's not just about preventing arthritis – it's about ensuring your joints work seamlessly throughout your life. Gut Health: It's More Than Just Digestion Now, let's shift our focus to the gut, often underestimated in its complexity. It's not just the place where food gets digested; it's a bustling hub of microbial activity, immune system coordination, and even mood regulation. And yes, it turns out that a happy gut can lead to happier joints. The Gut-Joint Connection: Unraveling the Mystery Inflammation: Gut health and joint health share a common enemy - inflammation. An imbalanced gut can lead to chronic inflammation, which in turn can affect joint tissues. Conditions like rheumatoid arthritis (RA) are closely tied to this inflammatory link. Immune System Modulation: Did you know that a significant portion of your immune system resides in the gut? A well-balanced gut microbiome helps regulate immune responses. When the gut is in harmony, it may reduce the risk of autoimmune conditions that target joints. Nutrient Absorption: Nutrients like vitamin D, calcium, and omega-3 fatty acids are crucial for joint health. The gut plays a pivotal role in absorbing these nutrients. An unhealthy gut may hinder their absorption, potentially impacting joint wellness. Microbial Metabolites: The gut microbiome produces metabolites that can influence inflammation and immune responses throughout the body, including the joints. Compounds like short-chain fatty acids (SCFAs) may have a protective effect on joints. Caring for Your Gut and Joints Now that we've seen the gut-joint connection, here are some friendly lifestyle tips to promote joint health through a happy gut: Diet: Incorporate a balanced diet rich in fiber, prebiotics, and probiotics to support a healthy gut microbiome. Include foods like yogurt, kefir, sauerkraut, and fiber-packed fruits and vegetables. Omega-3 Fatty Acids: Consider adding fatty fish, flaxseeds, and walnuts to your diet for their omega-3 content, which can have anti-inflammatory benefits for both your gut and joints. Bone-Building Nutrients: Consume foods rich in calcium and vitamin D, leafy greens such as kale, arugula, watercress, and collard greens and protein rich foods.. These nutrients are vital for strong bones and joints. Supplement with Collagen: The main protein found in bones is collagen. It contains the amino acids proline, glycine, and lysine, which help build bone, ligaments, muscle and tissues. Strength Training: Among the most effective forms of exercise to enhance bone health is weight-bearing or high-impact physical activity, as it stimulates the generation of new bone tissue. Stay Hydrated: Proper hydration is essential for joint health. Water helps lubricate joints and maintain their function. Consult a Professional: If you're experiencing joint issues, consult healthcare professionals who specialize in both gut and joint health. They can provide tailored advice and treatment options. In this article we've uncovered the remarkable connection between gut health and joint wellness. Remember, a happy gut can pave the way for happier joints, allowing you to enjoy a more flexible and active life. By nurturing your gut through a balanced diet, hydration, and professional guidance, you're taking a proactive step towards maintaining your joint health and overall well-being. So, here's to healthy joints and a thriving gut! As you navigate this path, know that I'm here to provide guidance, insights, and evidence-based strategies to help you unlock the potential of your gut for vibrant living. Your initial consultation is free and you can request it by clicking the button below: In the realm of health and wellness, the interconnection between various bodily systems often surprises us with its complexity. While we typically think of eye health as a standalone concern, emerging research has shed light on a fascinating relationship between the gut and the eyes. This connection underscores the importance of holistic health practices and highlights how nurturing your gut can potentially benefit your vision.
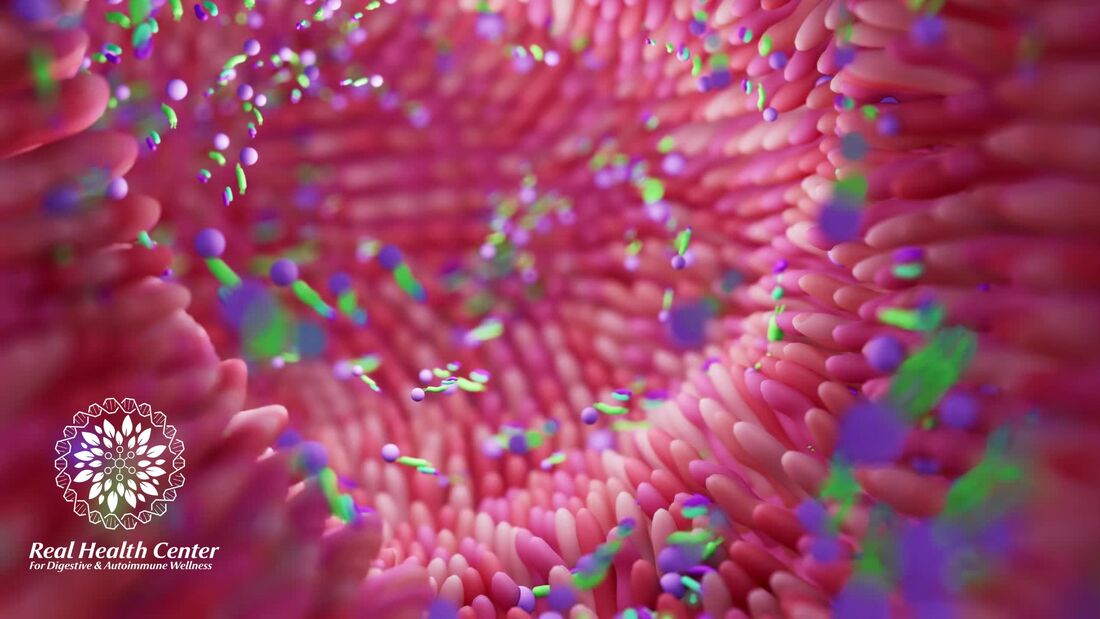
The Gut Microbiome: A Microscopic World with Macroscopic Implications The gut microbiome, a complex ecosystem of trillions of microorganisms residing in our digestive tract, plays a pivotal role in maintaining overall health. This collection of bacteria, fungi, viruses, and other microbes doesn't just aid in digestion; it influences various aspects of our well-being, including our immune system, metabolism, and now, it seems, our vision. Inflammation and Autoimmunity: Connecting the Dots Chronic inflammation and autoimmune diseases are known to wreak havoc on our body, and this includes our eyes. Conditions like uveitis and dry eye syndrome have been linked to systemic inflammation. The gut, being a central player in regulating inflammation, can either contribute to or mitigate this inflammation, depending on its health. The Gut's Role in Nutrient Absorption Nutrient deficiencies can have a profound impact on eye health. Key nutrients like vitamin A, lutein, zeaxanthin, and omega-3 fatty acids are essential for maintaining good vision. The gut is responsible for absorbing these nutrients from our food. An imbalanced gut microbiome can compromise nutrient absorption, potentially leading to eye problems. Microbial Balance and Immune Regulation A well-balanced gut microbiome supports a robust immune system. The immune cells in our gut are intricately connected to immune responses throughout the body, including in the eyes. Dysbiosis, an imbalance in gut microbes, can trigger inappropriate immune responses that may affect ocular tissues. The Gut-Brain-Eye Axis: A Fascinating Connection The gut-brain-eye axis is a burgeoning field of research. The vagus nerve, which connects the gut, brain, and eyes, plays a role in transmitting information between these organs. The gut can influence the brain, which in turn can influence vision. Stress, anxiety, and mood disorders associated with gut health can impact eye health. Promoting Gut and Eye Health Maintaining a healthy gut and supporting your vision involves a multifaceted approach: Diet: Consume a balanced diet rich in fiber, prebiotics, and probiotics to nurture your gut microbiome. Include foods high in eye-healthy nutrients like leafy greens, carrots, and fatty fish. Lifestyle: Manage stress through relaxation techniques and mindfulness, as chronic stress can negatively affect both gut and eye health. Supplementation: If necessary, consider supplements to bridge nutrient gaps, but always consult with a functional nutrition counselor first. Regular Check-ups: Visit your eye specialist and healthcare provider regularly to monitor your eye health and overall well-being. In conclusion, the connection between gut health and eye health is a fascinating area of study within the realm of functional medicine. While we are still uncovering the intricacies of this relationship, there is growing evidence to suggest that nurturing your gut can have a positive impact on your vision. Taking a holistic approach to health, one that includes proper nutrition, stress management, and gut support, may prove beneficial not only for your digestive system but also for the windows to your soul – your eyes. As you navigate this path, know that I'm here to provide guidance, insights, and evidence-based strategies to help you unlock the potential of your gut for vibrant living. Your initial consultation is free and you can request it by clicking the button below: The Gut-Body Symphony: Navigating the Intricate Connection Between Your Gut and Overall Health8/31/2023 Greetings to all those seeking a deeper understanding of holistic well-being! Today, we embark on an exploration of the wondrous and intricate connection that exists between your gut and the entire symphony of your body's functions. As a Certified Functional Medicine Practitioner and Functional Nutrition Counsellor, I am excited to guide you through the captivating realm of the gut-body connection.
A Microbial Tapestry: The Gut Microbiome Picture your gut as a thriving ecosystem bustling with life—a tapestry woven from trillions of microorganisms collectively known as the gut microbiome. This vibrant community of bacteria, yeasts, and other microbes plays a pivotal role in not only your digestive health but also your overall vitality. Beyond Digestion: A Multifaceted Influence While the gut's primary role is digesting and absorbing nutrients from the foods you consume, its influence extends far beyond the confines of the digestive process. The gut microbiome holds the key to several aspects of your well-being: 1. Immune Function: A significant portion of your immune system resides in the gut. The gut microbiome and immune system communicate in a dynamic dance, shaping the body's immune responses. A harmonious gut microbiome contributes to a robust immune defense against pathogens and harmful invaders. 2. Hormonal Balance: Surprisingly, your gut microbiome can influence hormonal balance. Microbes participate in metabolizing hormones like estrogen, impacting their levels and potentially influencing menstrual cycles, mood, and hormonal health. 3. Brain-Gut Axis: The gut-brain connection is a fascinating bridge between your gut and your central nervous system. This bidirectional communication influences mood, cognition, and mental well-being. The gut microbiome produces neurotransmitters and communicates with the brain through neural and hormonal pathways. 4. Nutrient Synthesis: Certain gut bacteria play a role in synthesizing vitamins and other nutrients, contributing to your overall nutrient status. 5. Metabolic Health: The gut microbiome can impact your metabolism, affecting how your body processes and stores energy. Imbalances in the microbiome have been linked to metabolic disorders like obesity and type 2 diabetes. 6. Inflammation Regulation: A harmonious gut microbiome can help regulate inflammation—a vital response that, when dysregulated, can lead to chronic health conditions. Nurturing the Gut-Body Harmony As you navigate the landscape of holistic health, nurturing the gut-body connection emerges as a cornerstone. Here's how you can promote a thriving gut microbiome and unlock its multifaceted benefits: 1. Fiber-Rich Diet: Embrace a diet rich in fiber from whole grains, fruits, vegetables, and legumes. Fiber nourishes beneficial gut bacteria and supports their growth. 2. Diverse Foods: Encourage microbial diversity by consuming a variety of plant-based foods. Each type of fiber feeds different groups of bacteria. 3. Probiotic Foods: Incorporate fermented foods like yogurt, kefir, sauerkraut, and kimchi to introduce beneficial bacteria into your gut. 4. Prebiotic Foods: Consume prebiotic-rich foods like garlic, onions, and bananas. These foods provide nourishment for your existing gut bacteria. 5. Hydration and Mindful Eating: Stay hydrated and practice mindful eating to support optimal digestion and nutrient absorption. 6. Stress Management: Chronic stress can impact the gut microbiome. Engage in stress-reducing activities such as meditation, yoga, and spending time in nature. 7. Professional Guidance: Collaborate with functional medicine practitioners to tailor a holistic plan that nurtures your gut and aligns with your unique health profile. In conclusion, the gut-body connection is a captivating journey of discovery that underscores the interplay between your gut microbiome and your overall well-being. By nurturing your gut, you're nurturing every facet of your health. As you navigate this path, know that I'm here to provide guidance, insights, and evidence-based strategies to help you unlock the potential of your gut for vibrant living. Your initial consultation is free and you can request it by clicking the button below: Gastritis, a condition that involves inflammation of the stomach lining, can bring discomfort and challenges to daily life. Understanding its intricacies and adopting a holistic approach to treatment can pave the way for effective relief and lasting healing. In this article, we'll explore the various facets of gastritis and delve into a robust holistic treatment plan that encompasses dietary adjustments, lifestyle modifications, natural remedies, and long-term strategies.
Unraveling the Complexity of Gastritis Gastritis isn't a one-size-fits-all condition; it presents itself in different forms, including acute, chronic, erosive, and non-erosive. To effectively address it, it's essential to comprehend its underlying causes and triggers. Various factors contribute to gastritis, including H. pylori infection, stress, certain medications, alcohol consumption, smoking, and dietary choices. This multifaceted nature underscores the need for a comprehensive treatment approach. Empowering Your Diet for Healing A cornerstone of gastritis management lies in dietary adjustments. The adoption of an anti-inflammatory diet can work wonders in reducing stomach inflammation and alleviating symptoms. Prioritizing whole, unprocessed foods and steering clear of triggers such as spicy, acidic, and fatty foods is paramount. Incorporating herbs and spices known for their anti-inflammatory properties can further enhance the healing potential of your diet. Nurturing Gut Health Through Foods and Supplements Promoting gut healing is a central objective in the management of gastritis. Certain foods and supplements can aid in this process. Probiotics and prebiotics play a crucial role in maintaining a balanced gut microbiome, while nutrient-rich options like bone broth, aloe vera, and specific vitamins and minerals offer support to the stomach lining and facilitate digestion. Harnessing the power of these nutritional elements contributes to a holistic approach. Harmonizing Lifestyle for Balance Stress management holds a key position in alleviating gastritis symptoms. Techniques such as mindfulness, meditation, and relaxation exercises can effectively reduce stress and create a sense of equilibrium. Additionally, paying attention to sleep, hydration, and exercise contributes to overall gut health. Embracing these lifestyle modifications can foster a comprehensive approach to gastritis relief. Exploring Nature's Remedies Natural remedies have long been valued for their potential to alleviate discomfort and promote healing. Ginger, turmeric, chamomile, and licorice root are among the natural allies that can help reduce inflammation, soothe stomach distress, and provide relief from symptoms. Integrating these remedies into your routine can offer a complementary layer of support. Soothing with Herbal Teas and Infusions Incorporating herbal teas and infusions into your routine can provide gentle comfort for gastritis symptoms. Crafted to deliver a soothing effect on the stomach and digestive system, these warm concoctions offer both physical relief and a sense of well-being during the healing journey. Balancing Medical Interventions and Holistic Approaches While holistic strategies are pivotal, acknowledging the potential need for medical interventions is also important. Collaborating with healthcare providers to explore options such as medications and medical procedures can offer relief when necessary, aligning with a comprehensive approach to care. Embracing Long-Term Healing Gastritis demands commitment for lasting relief. Transitioning from acute symptom management to a phase of maintenance and prevention is essential for ongoing well-being. By maintaining dietary adjustments, lifestyle modifications, and a holistic perspective, individuals can chart a course towards long-term healing and optimal gut health. In conclusion, gastritis is a multifaceted condition that requires a holistic approach for effective relief and healing. By understanding its nuances and adopting a comprehensive plan that encompasses diet, lifestyle, natural remedies, and potential medical interventions, individuals can embark on a journey towards lasting well-being. Customizing your approach and making informed decisions will be key as you navigate the path to relief and healing. Your initial consultation is free and you can request it by clicking the button below: Greetings to all seekers of holistic health! Today, we embark on a journey into the realm of your gut, where an intricate dance between bacteria and inflammation unfolds. As a Certified Functional Medicine Practitioner and Functional Nutrition Counsellor, I am excited to explore the profound connection between bacterial overgrowth, inflammation, and its wide-ranging impact on your body.
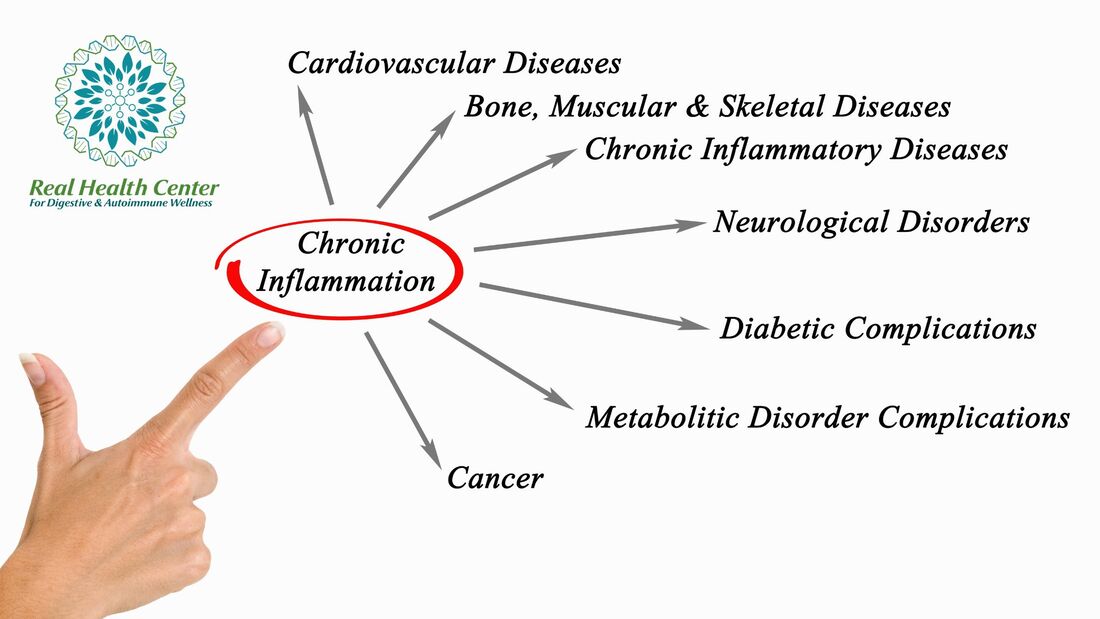
The Hidden Player: Bacterial Overgrowth In the intricate landscape of your gut, bacterial overgrowth can cast a shadow over the delicate balance of your microbiome. This overgrowth can trigger a cascade of events, including inflammation, that extends beyond the confines of your digestive system. Inflammation: The Double-Edged Sword Inflammation is your body's natural response to harmful stimuli, such as infections or injuries. However, when inflammation becomes chronic and systemic—persisting even when there is no real threat—it can wreak havoc on your health. Bacterial overgrowth in the small intestine can fuel this chronic inflammation, initiating a cycle that affects your entire body. The Gut Inflammation Connection Bacterial overgrowth triggers inflammation in the gut through various mechanisms. For instance, as bacteria ferment undigested food particles, they produce metabolic byproducts that can irritate and damage the gut lining. This irritation prompts an immune response, leading to inflammation in the gut tissues. Systemic Impact of Inflammation Here's where the story takes an intriguing turn. Inflammation that starts in the gut doesn't necessarily stay there. It has the potential to travel throughout your body via the bloodstream. This phenomenon, known as "systemic inflammation," is a key player in the development of various health conditions. The Domino Effect on Health Conditions Cardiovascular Disease: Chronic inflammation can damage blood vessels and contribute to the formation of arterial plaques, increasing the risk of heart disease, stroke, and other cardiovascular issues. Autoimmune Disorders: Systemic inflammation can trigger or exacerbate autoimmune conditions, where the immune system mistakenly attacks healthy tissues. Disorders like rheumatoid arthritis, lupus, and inflammatory bowel disease have strong ties to inflammation. Metabolic Syndrome: Inflammation can disrupt insulin sensitivity and contribute to metabolic syndrome—a cluster of conditions including obesity, high blood pressure, and insulin resistance. Neurological Impact: Emerging research suggests a link between chronic inflammation and neurological conditions like Alzheimer's disease and Parkinson's disease. Cancer Risk: Chronic inflammation can create an environment conducive to cancer development, promoting cellular changes and genetic mutations. Empowering Your Health Journey Understanding the link between bacterial overgrowth, gut inflammation, and systemic health enables you to take proactive steps towards well-being: Gut-Nourishing Foods: Opt for an anti-inflammatory diet rich in whole foods, leafy greens, fatty fish, nuts, and antioxidant-rich fruits. Healthy Fats: Incorporate omega-3 fatty acids found in flaxseeds, chia seeds, and fatty fish. These fats have anti-inflammatory properties. Probiotics and Prebiotics: Promote a balanced gut microbiome by consuming probiotic-rich foods (yogurt, kefir) and prebiotic foods (garlic, onions, bananas) that fuel beneficial bacteria. Stress Management: Chronic stress can fuel inflammation. Prioritize relaxation techniques like meditation, yoga, and deep breathing. Professional Guidance: Collaborate with professionals who specialize in functional medicine to create a personalized plan that addresses inflammation and its effects. Remember, the journey to vibrant health is a collaborative effort. By addressing bacterial overgrowth and inflammation, you're taking a significant step towards a balanced and harmonious well-being. Your initial consultation is free and you can request it by clicking the button below: Welcome to a new dimension of wellness where the intricate dance between your gut health and nutrient absorption takes center stage. As a Certified Functional Medicine Practitioner and Functional Nutrition Counsellor, I'm excited to share how disruptions in your gut health, particularly bacterial overgrowth, can lead to a chain reaction affecting your nutrient absorption and, subsequently, your overall health.
The Silent Culprit: Bacterial Overgrowth Picture your small intestine as a gatekeeper responsible for allowing essential nutrients to enter your bloodstream. Bacterial overgrowth, however, can disrupt this delicate process. When the population of gut bacteria becomes imbalanced, it can interfere with the absorptive surface of the small intestine, hindering its ability to extract nutrients from the food you consume. The Nutrient Deficiency Domino Effect When your small intestine struggles to absorb nutrients properly, it sets off a chain of events that reverberates throughout your body. Nutrient deficiencies can impact various bodily functions, giving rise to a myriad of health concerns: Anemia: Insufficient absorption of iron, vitamin B12, and folic acid can lead to anemia, a condition characterized by reduced red blood cell production and oxygen transport. Anemia can result in fatigue, weakness, and impaired cognitive function. Bone Health: Calcium and vitamin D absorption are crucial for maintaining strong and healthy bones. Bacterial overgrowth-related nutrient deficiencies could contribute to weakened bones, potentially increasing the risk of fractures and osteoporosis. Immune System Weakness: Micronutrients like zinc, selenium, and vitamins A and C are essential for a robust immune system. Deficiencies in these nutrients can compromise your body's defense mechanisms, leaving you more susceptible to infections. Neurological Implications: Nutrients such as vitamin B6, B12, and folate play pivotal roles in nerve function and neurotransmitter synthesis. Inadequate absorption can lead to neurological symptoms like numbness, tingling, and cognitive disturbances. Skin Health: Nutrient deficiencies can manifest on your skin, causing issues like dryness, flakiness, and reduced wound healing. The Path to Restoration Understanding the connection between bacterial overgrowth, nutrient absorption, and overall health underscores the importance of nurturing your gut. Here's how you can embark on a journey to restore nutrient harmony: Balanced Diet: Prioritize nutrient-dense foods rich in vitamins, minerals, and antioxidants. Incorporate a variety of fruits, vegetables, lean proteins, and whole grains. Gut-Friendly Foods: Integrate foods that promote gut health, such as fermented foods (yogurt, kefir, sauerkraut) and high-fiber options (beans, legumes, whole grains). Digestive Enzymes: In some cases, digestive enzyme supplements can aid nutrient absorption by breaking down food components more effectively. Professional Guidance: Collaborate with a natural health professional who understands functional medicine and can guide you through tailored dietary and supplement recommendations. Mindful Eating: Practice mindful eating habits to support digestion. Chew your food thoroughly, eat in a relaxed environment, and avoid rushing through meals. By nurturing your gut health, you're not only optimizing nutrient absorption but also laying a foundation for overall well-being. Remember, each individual's gut health is unique, and personalized guidance is key to achieving your health goals. As you embark on this journey, know that I'm here to provide support, guidance, and evidence-based insights. Let's unlock the potential of your gut for optimal health together. Your initial consultation is free and you can request it by clicking the button below: |
AuthorAyesha Syed, AFMC is a Certified Functional Medicine Practitioner and a Certified Functional Nutrition Counsellor. At the Real Health Center, she helps you manage Autoimmune Health and Digestive/GI Health applying functional medicine principles and testing if needed, nutritional counseling, lifestyle, and complementary therapies designed to support your overall health and balance. Archives
July 2024
Categories
All
|








 RSS Feed
RSS Feed