|
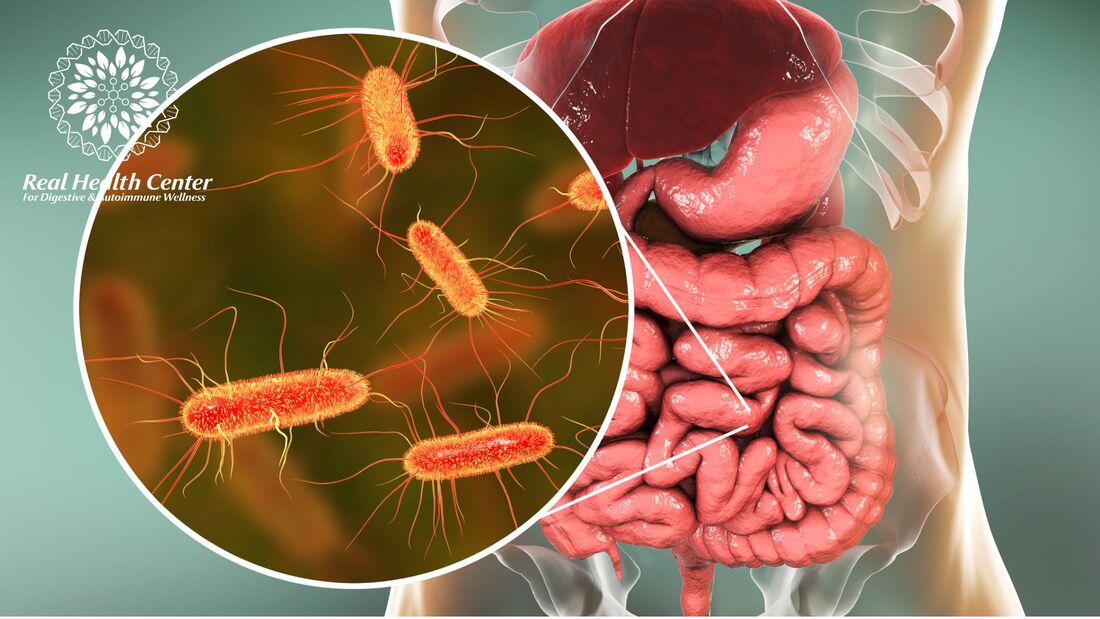
Bacterial overgrowth in the small intestine can have broader implications for health beyond just digestive discomfort. This concept is rooted in the understanding that the gut microbiome plays a pivotal role in overall well-being, and disturbances in gut health can potentially impact various body systems. Here's an overview of the connection between digestive issues and other health conditions:
Gut-Body Connection: The gut microbiome, which includes various types of bacteria, can influence not only digestive health but also immune function, hormonal balance, and even mental well-being. Systemic Inflammation: Bacterial overgrowth in the small intestine can lead to increased inflammation in the gut. This localized inflammation can have systemic effects, potentially contributing to chronic inflammation throughout the body. Chronic inflammation is known to be a factor in a wide range of health conditions, including cardiovascular disease, autoimmune disorders, and metabolic syndrome. Immune System Modulation: The gut is a significant part of the body's immune system. An imbalance in gut bacteria can disrupt the delicate balance of the immune response, potentially leading to immune-related conditions and allergies. Bacterial overgrowth may negatively influence immune system function. Nutrient Absorption and Deficiencies: When the small intestine's ability to properly absorb nutrients is compromised due to bacterial overgrowth, it can lead to nutrient deficiencies. These deficiencies can affect various bodily functions, potentially contributing to health issues ranging from anemia to compromised bone health. Hormonal Imbalances: Gut health has been linked to hormonal regulation. An imbalanced gut microbiome can impact the production and metabolism of hormones, potentially contributing to hormonal imbalances that affect reproductive health, mood, and more. Neurological and Mental Health: The book also touches on the emerging field of the gut-brain connection. Disruptions in gut health, such as bacterial overgrowth, could influence neurotransmitter production and communication between the gut and the brain. This connection has implications for mental health conditions like anxiety and depression. Autoimmune Conditions: There’s a potential role of gut health in autoimmune diseases. While the exact mechanisms are complex and not fully understood, there is growing evidence suggesting that imbalances in gut bacteria may contribute to triggering or exacerbating autoimmune conditions. Metabolic Health: Disturbances in gut microbiota composition and function have been linked to metabolic disorders such as obesity and insulin resistance. Addressing gut health could potentially play a role in managing metabolic conditions. It's important to note that the connections between gut health and these various health conditions are areas of ongoing research, and the exact mechanisms involved are complex and multifaceted. The above points highlight these potential links to emphasize the importance of addressing bacterial overgrowth not only for digestive comfort but also for overall health and well-being. As a Certified Functional Medicine Practitioner and Functional Nutrition Counsellor, I inform and educate my clients about the broader implications of gut health and guide them toward approaches that promote a balanced gut microbiome. In my practice, I approach each client's health journey holistically and consider collaborating with other healthcare professionals when necessary. Your initial consultation is free and you can request it by clicking the button below:
0 Comments
|
AuthorAyesha Syed, AFMC is a Certified Functional Medicine Practitioner and a Certified Functional Nutrition Counsellor. At the Real Health Center, she helps you manage Autoimmune Health and Digestive/GI Health applying functional medicine principles and testing if needed, nutritional counseling, lifestyle, and complementary therapies designed to support your overall health and balance. Archives
September 2023
Categories
All
|

 RSS Feed
RSS Feed